Welcome to
Welcome to
Tinsley Surgical
Tinsley Surgical
Ready to improve your health? Take the first step!
Click to get your appointment and begin your wellness journey with us.
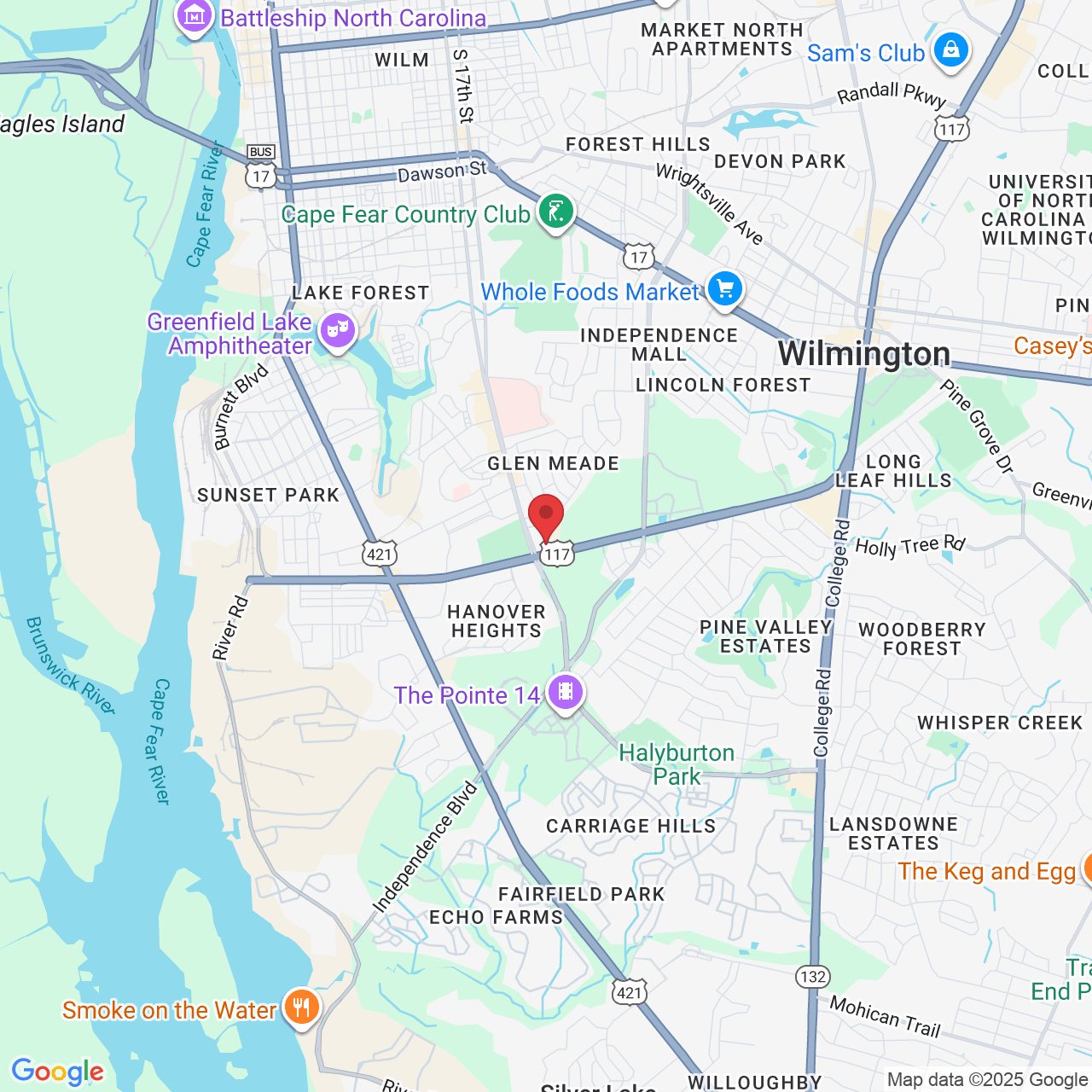
Office:
1717 Shipyard Boulevard Suite 200
Wilmington, NC 28403
Call (910) 769-2583
Email: [email protected]
Conditions We Can Help
What We Treat
Tinsley Surgical
What to Expect
At Tinsley Surgical, our dedicated team is committed to providing expert care for a wide variety of medical conditions. Our comprehensive approach ensures that you receive the best possible treatment for your specific needs. Whether you're struggling with vein or vascular issues, or you require general surgery for other health concerns, we have the expertise and advanced techniques to help you regain your health and well-being.
"NICE TO MEET YOU"
Meet Our Team

Tinsley Surgical is a well-known and highly respected vein, vascular, and general surgery practice in Wilmington, North Carolina.
Headed by Ellis A. Tinsley, Jr., MD, FACS, FSVS, the Tinsley Surgical team strives to help patients live comfortably and with confidence!
Dr. Tinsley brings with him years of experience and myriad satisfied customers. He and his team take time to understand each client’s needs and treat every consult with meticulous attention to detail and unmatched professional expertise. The result is fast, effective, and lasting vein and vascular surgical solutions.
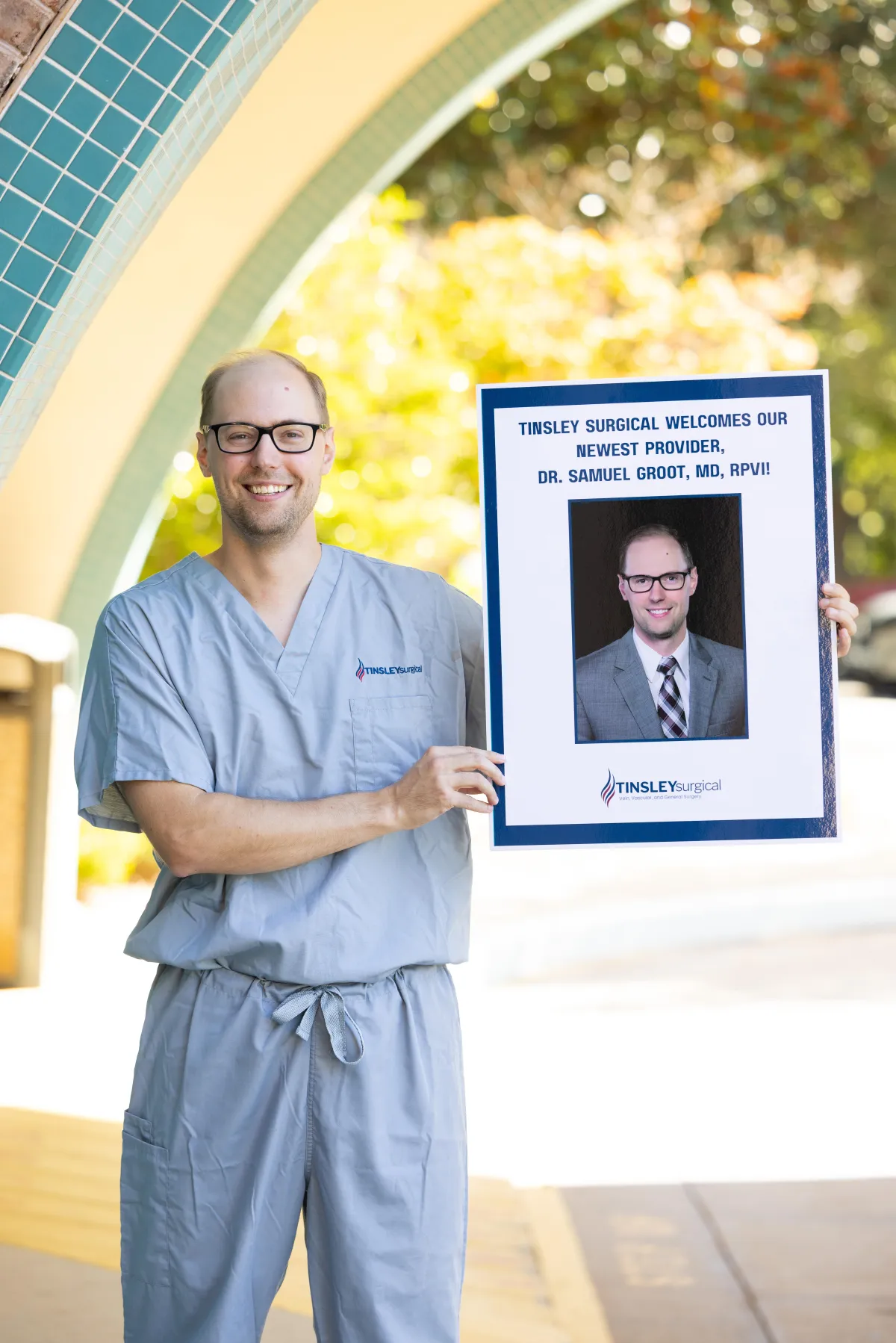
Joining the team at Tinsley Surgical is Samuel J. Groot, MD, RPVI, a board-certified vascular surgeon specializing in carotid, aortic, arterial, and venous care.
Dr. Groot completed his fellowship at the Midwest Aortic & Vascular Institute and residency at Prisma Health Upstate South Carolina, following his medical degree from Texas Tech University School of Medicine and undergraduate studies at Baylor University. His expertise includes carotid disease (endarterectomy and TCAR), aortic disease, peripheral artery disease, and venous disease.
Dr. Groot shares the same patient-first philosophy as the rest of the Tinsley Surgical team, providing the same level of care and compassion he would want for his own family. His addition expands the practice’s ability to deliver advanced vascular and surgical care to the Wilmington community with precision, safety, and exceptional results.
Testimonials
See What Patients Are Saying
LET'S TALK
CONTACT US HERE
Get In Touch
Email: [email protected]
Address
Office: 1717 Shipyard Boulevard Suite 200
Wilmington, NC 28403
Business Hours
Mon - Fri 8AM - 5:00 PM
Saturday - CLOSED
Sunday - CLOSED
Phone Number:
(910) 769-2583